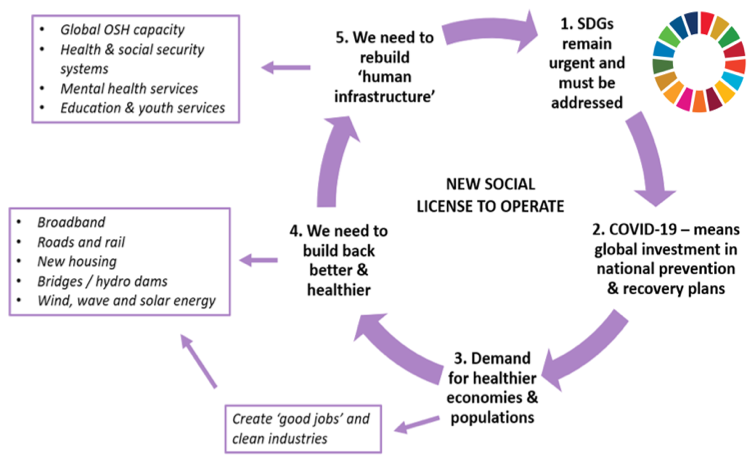
As the ‘Decade of Action’ (2020-30) for the United Nations Sustainable Development Goals (SDGs) grows in urgency, what should it mean for occupational safety and health (OSH) and ensuring that allwork is good work? How do we best address the needs of a virus-affected world and the challenges and opportunities of the 4thIndustrial Revolution, the digital and green economies, demographic and technological changes, and the future of work? How do we ensure that we revitalise our support systems and ‘build back better and healthier’?
Many of the SDGs relate to work and to OSH, as highlighted in the IOSH sustainability policy, particularly SDG Goal 3 ‘Ensure healthy lives and promote wellbeing for all at all ages’ and SDG Goal 8 ‘Promote sustained, inclusive and sustainable economic growth, full and productive employment and decent work for all’, which includes ending modern slaveryand human trafficking.
Importantly, as we’ve all witnessed, the Coronavirus pandemic has reinforced the intrinsic links between environmental, public, occupational and general health, as well as shining a light on health inequalities and the need to better protect health and social care workers and others on the frontline, and to ‘build back better and healthier’. This includes ensuring effective test, trace and isolate systems, and access to personal protective equipment, vaccines, therapeutics and ongoing mental health support. Central to delivering improvement is SDG Goal 17 ‘Strengthen the means of implementation and revitalise the global partnership for sustainable development’. This UN call for international capacity-building and multi-stakeholder partnerships to ‘mobilise and share knowledge’ is a clear request for stronger multidisciplinary working and for all health and health-related professionals to contribute.
This is where I believe the collective health community, professional bodies and networks have pivotal roles, both now and in the future. We need to see OSH / OH professionals increasingly harnessed to help public policymakersand organisations tackle the complex work-related health challenges, such as from climate change, air pollution and extreme weather; increased sedentarianism; extended working lives; the needs of workers with health conditions and disabilities; tackling communicable and non-communicable diseases at work; and the exponential growth in new workplace technology, automation and artificial intelligence.
We need to work together to ensure greater focus on human-centred public- and corporate-policy and on managing psychosocial risk at work, with mental healthfinally gaining parity with physical health, and stigma ended. And we need to collaborate to support diverse and inclusive workforces, protect vulnerable groups and embed OSH risk-intelligence as a key life- and employment-skill, essential to long-term social value and achieving SDG Goal 4 ‘Ensure inclusive and equitable quality education and promote lifelong learning opportunities for all’.
Thankfully, in the decade ahead, I think we can expect to see better-informed public opinion continue to drive higher societal expectationsand requirements on organisations and leaders seeking new ‘social licenses’ to operate and govern. And also see improved performance evaluation and transparency increasingly sought by stakeholders wanting assurance, not only that no-one is being harmed by public policy or corporate activity, but that people’s health and wellbeing is actively enhanced in line with our more socially conscious world.
This demand for transparency and comprehensive corporate reportingwill help drive meaningful and comparable OSH performance reportingat global, national and corporate levels and recognition that good OSH must be a fundamental right worldwide. Professionals have key parts to play, fostering positive and learning cultures; designing-in OSHand evaluating interventions; developing meaningful indicators and utilising data; and making recommendations to improve OSH performance across regions, organisations and supply chains.
So, what key changes are needed to tackle the millions of work-related deaths each year, improve OSH and wellbeing and deliver on the SDGs? I believe they must include:
- Recognising OSH as essential to public and socioeconomic good, so that it is designed into all public-policy,global trade, international development and corporate strategies
- Building global OSH capacityand improving access worldwide, including for micros, SMEs, the self-employed, migrant and informal workers and all those on the frontline
- Harmonising and standardising meaningful OSH performance reportingto drive global, national and corporate decision-making and investment for prevention, emergency planning and improved OSH and wellbeing
To close, can I just urge that, as professionals, influencers and networks, we continue working together and reaching out to ensure that this decade is one in which the true value of OSH / OH is harnessed to support good work for all, healthier populations and sustainable futures.
If you’d like to know more and support IOSH’s advocacy work on ‘building back better and healthier’, please contact the IOSH Policy team at publicaffairs@iosh.com.
Richard Jones
IOSH
13 November 2020














